- Home
- About Us
- Why BFI
- Treatments
Advanced IVF Treatment
Donor Services
Fertility Preservation
Advanced IVF Treatment
Donor Services
Fertility Preservation
- Locations
- Resources
- Contact Us
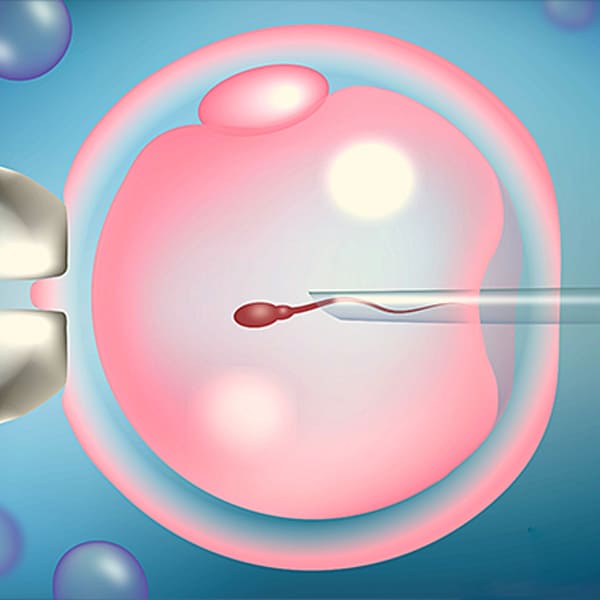
ICSI Treatment (Intracytoplasmic Sperm Injection)
ICSI is the miraculous game-changer technique where only ONE SPERM is required to fertilize ONE EGG. ICSI changed the fertilization process in IVF and made IVF successful even in otherwise impossible situations.
ICSI is a part of IVF treatment and used for fertilization. Hence, IVF and ICSI are not two different treatments.
Fertilization is the most crucial step in reproduction. In natural fertilization, millions of sperm are required to achieve successful fertilization. Hence, the normal considered sperm count is 15 million per ML.
In conventional IVF, the process of fertilization is done by putting an egg and a few hundred sperm in a droplet/small quantity of culture medium. Then we wait for the sperm to fertilize the egg. Fertilization of the egg by sperm is a very complex process. It requires sperm’s or egg’s capacity to do this process successfully.
Occasionally with conventional IVF, we see fertilization failure or very poor fertilization. Sperm quantity and quality are often severely compromised for use with conventional IVF, and ICSI is required.
After the advent of ICSI, the problem of fertilization is resolved to a very great extent. All good IVF clinic that has the technology and in house skilled embryologist, prefer ICSI for all.
BFI performs “ICSI for all” when it comes to fertilization. Our latest generation of automated ICSI machines gives us precision in microns to help our expert and experienced embryologist deliver the best fertilization rates.
ICSI is a short form for
- Intra – Inside
- Cytoplasmic – Cytoplasm of oocyte- egg
- Sperm – Male gamete – sperm
- Injection – Injection
HOW IS ICSI DONE?
Sperm are specially prepared for easy handling for ICSI. A special microscope is used to see the sperm in high magnification for minute details. In ICSI, the best sperm are first selected based on their motility and structure in the microscope. The sperms are activated by snapping their tail by the micromanipulation technique. This trigger final changes in the sperm that it achieves when binding with the oocyte; it is also known as acrosome reaction. One sperm is then introduced into the egg with a special microneedle. Thus, fertilization is almost achieved. Egg damage with ICSI is very uncommon.
Only one sperm is required to fertilize one egg, not millions!
ICSI FOR WHOM?
ICSI gives better fertilization compared to conventional IVF translating into better pregnancy rates. So almost all cycles of IVF at Bavishi Fertility Institute are ICSI cycles! Sperm with very poor fertilizing capacity also can be used with ICSI.
ICSI is especially needed for:
Men with low sperm quality
- Low sperm concentration,
- Poor motility
- Poor morphology
- Frozen sperm
- Very less available quantity
- Previous fertilization failure
- Sperm recovered from testis or epididymis
- Patients with azoospermia
- Patients who have had a vasectomy
Women who may benefit more
- Very less eggs
- Poor quality eggs
- Previous fertilization failure with conventional IVF
- Advanced age
Couples with unexplained infertility also can benefit from ICSI by preventing unexplained fertilization failure.
ADVANTAGE BFI
Get the advantage of our experience of thousands of cycles and perfected technique.
Book an appointment now!

