- Home
- About Us
- Why BFI
- Treatments
Advanced IVF Treatment
Donor Services
Fertility Preservation
Advanced IVF Treatment
Donor Services
Fertility Preservation
- Locations
- Resources
- Contact Us
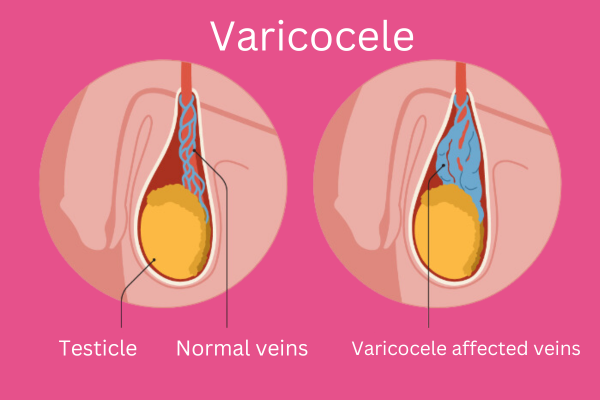
What is Varicocele?
Varicocele is a condition that occurs when the veins in the scrotum, the pouch of skin that holds the testicles, become enlarged. These enlarged veins are similar to varicose veins that can develop in the legs.They are usually painless and don’t cause any problems. However, in some cases, varicoceles can cause scrotal pain or infertility.
Varicoceles are thought to be caused by a weakness in the valves of the veins in the scrotum. These valves normally help to keep blood flowing in one direction, back towards the heart. When the valves are weak, blood can pool in the veins, causing them to enlarge.
What are the grades of a varicocele?
Grade I (Subclinical or Small): This grade is characterized by a varicocele that can only be felt when you press on it during a Valsalva maneuver (like when you strain or cough). It’s not easily felt when you’re not pressing on it.
Grade II (Moderate): A Grade II varicocele is easy to feel without pressing on it. You can notice the swelling of veins by touching the scrotum.
Grade III (Large or Severe): This grade represents a varicocele that is not only easy to feel without pressing, but you can also see it because the veins are significantly swollen.
Symptoms of Varicocele
Varicoceles often do not cause any symptoms. However, some men may experience:
- Dull, aching pain or discomfort in the scrotum, particularly after standing for long periods.
- Visible or palpable enlargement of the veins in the scrotum.
- Shrinking of the affected testicle (in rare cases).
Causes of Varicocele
The exact cause of varicoceles is not always clear, but several factors are believed to contribute to their development. Here are some potential causes of varicoceles:
- Faulty valves in the spermatic veins
- Genetic predisposition
- Abnormal blood flow
- Increased pressure in the abdomen
- Hormonal factors
- Nutritional factors
Complications of Varicocele
While varicoceles are generally considered harmless, they can lead to complications such as:
- Infertility: Varicoceles may contribute to male infertility by causing a decline in sperm quality.
- Testicular Atrophy: In rare cases, untreated varicoceles can result in the shrinking of the testicles.
How is a Varicocele diagnosed?
A varicocele is typically diagnosed through a combination of medical history, physical examination, and imaging studies. Here’s an overview of the diagnostic process:
- Medical History: The doctor will ask questions about your symptoms, such as pain or discomfort in the scrotum, fertility concerns, or changes in testicle size. They may inquire about your overall health, medical history, and any previous surgeries or treatments.
- Physical Examination: A physical examination is a crucial step in diagnosing a varicocele. The doctor will examine the scrotum while you are standing and lying down to detect any swelling or enlargement of the veins in the spermatic cord. They may perform a Valsalva maneuver, where you are asked to bear down as if having a bowel movement, to help identify the varicocele. Clinically identified varicocele may need treatment depending on semen parameters .
- Imaging Studies: Doppler ultrasound is the most common imaging test used to diagnose varicoceles. The ultrasound helps visualize the blood flow in the veins of the scrotum, allowing the doctor to identify any dilated or enlarged veins. Ultrasound can also help determine the severity of the varicocele and whether it might be affecting blood flow to the testicles. Grade 3/4 varicocele diagnosed by doppler may need treatment if semen report is abnormal.
How is a Varicocele treated?
Treatment options for varicocele may vary depending on the severity of symptoms, the presence of fertility issues, and the overall health of the individual. Here are some common approaches to treat varicocele:
- Observation: In some cases, especially if the varicocele is small and not causing significant symptoms, a healthcare provider may recommend a “wait-and-see” approach. Regular monitoring may be suggested to check for any progression in the condition.
- You may consider semen freezing to preserve the sperm quality if planning for this mode of management.
- Lifestyle modifications: Making certain lifestyle changes, such as avoiding prolonged periods of sitting or standing, avoiding heat exposure to testis, wearing supportive underwear, and practicing good genital hygiene, can help alleviate discomfort associated with varicocele.
- Surgical treatment:
Varicocelectomy: This is a surgical procedure in which the affected veins are ligated or removed. There are different techniques for varicocelectomy, including open surgery, laparoscopic surgery, and microsurgery. Usally microsurgical approach is considered the best.This procedure is often considered if the varicocele is causing pain, discomfort, or fertility issues.Assisted reproductive techniques (ART): If the varicocele is associated with male infertility, assisted reproductive techniques such as in vitro fertilization (IVF) or intrauterine insemination (IUI) may be considered. Surgical treatment may not be suitable for some patients, Some patients who don’t like to undergo surgery; ART is a good treatment option for these patients.
How to prevent Varicocele?
While it may not be possible to prevent varicoceles entirely, some measures may help reduce the risk of developing them:
- Avoiding prolonged periods of standing or sitting, which can increase pressure in the veins of the scrotum.
- Avoid excessive heat exposure to genitelia. Avoid placing laptops or computers in lap. Avoid regular sauna and steambath.
- Wearing supportive underwear, such as briefs or athletic supporters, to provide additional support to the scrotum and reduce pressure on the veins.
- Maintaining a healthy lifestyle, including regular exercise and a balanced diet, to promote overall vascular health.
FAQs
If left untreated, varicoceles may not necessarily cause significant health problems. However, they can potentially lead to infertility or testicular atrophy in rare cases. It is essential to discuss the potential risks and benefits of treatment with a healthcare provider.
The decision to treat a varicocele in adolescents depends on various factors, including the size of the varicocele, symptoms, and potential impact on fertility. It is advisable to consult with a pediatric urologist or reproductive specialist to determine the appropriate course of action. If worried about future reproductive issues semen freezing may be considered.
If you are asymptomatic but concerned about fertility issues, it may be worthwhile to undergo an evaluation to assess sperm quality and reproductive function. Depending on the findings, varicocele repair may be considered as part of a comprehensive fertility treatment plan.
The time it takes to see improvements in semen quality following varicocele repair can vary from individual to individual. In some cases, improvements may be observed within a few months, while in others, it may take longer. Earliest improvement is seen after 2-3 months. One year after surgery there are very rare chances of further improvement in semen parameters. It is essential to follow up with a healthcare provider for regular semen analysis to monitor progress.
Varicoceles are typically not considered life-threatening, but they can have implications for fertility and testicular health. You may consider semen freezing to preserve the sperm quality if not planning to conceive in a reasonable amount of time. While some varicoceles may remain asymptomatic and require no treatment, others may cause discomfort or contribute to infertility. It is essential to seek medical advice for proper evaluation and management.
Varicoceles are unlikely to affect physical growth or development.
Recovery time varies:
- Open surgery: A few weeks
- Minimally invasive procedures: About a week or two
- Observation: No specific recovery period
No, varicoceles typically don’t cause erectile dysfunction. Consult a healthcare provider for concerns about sexual function.
